Data Integration for Public Health Action
July 31, 2025
3 min read 559 wordsWhen data lives in silos, opportunities are missed. A connected picture—built from surveillance, EHR, registries, and program data—helps leaders act faster and fairer. Start by deciding which outcomes and decisions you want to support; the checklist in choosing outcomes that matter keeps scope tight. Because integrated systems rely on routine data, set expectations with real‑world evidence in healthcare decision‑making and keep inputs trustworthy using EHR data quality for real‑world evidence.
A pragmatic roadmap
- Define purpose and use cases
- Target 2–3 decisions (e.g., early warnings for maternal complications; preventive outreach for asthma; overdose cluster detection).
- Write plain‑language outcome definitions and owners.
- Map sources and plan matching
- Sources: surveillance events, EHR encounters, registries, vital records, program rosters, claims.
- Matching: deterministic where possible (national IDs, MRNs) with strict format rules; fuzzy matching fallback with thresholds and clerical review.
- Report match rates and uncertainty. Publish “data notes” for anomalies.
- Build minimal‑viable metadata (MVM)
- For each dataset: owner, refresh cadence, field dictionary, code systems, units, known gaps.
- Standardize 10–20 core fields across sources (IDs, dates, codes, units, language preference, interpreter need).
- Governance and agreements
- Data sharing and processing agreements with clear purposes, retention, and redress.
- Role‑based access; audit logs; incident response with time‑bound commitments.
- Community oversight where appropriate.
- Privacy‑by‑design
- Separate identifiers; tokenize where feasible; encrypt in transit and at rest.
- Opt‑in for sensitive topics; minimize collection; provide correction/opt‑out paths.
- Follow reproductive‑health guardrails echoed in AI‑supported contraceptive counseling.
- Deliver value early
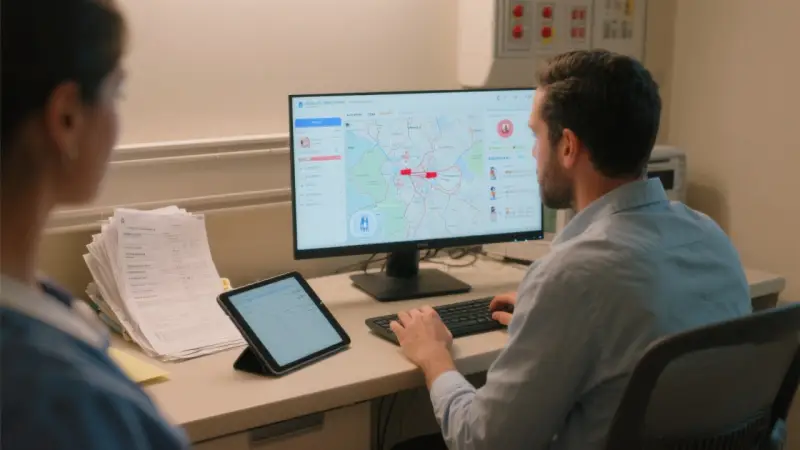
- One‑page dashboards for the first two use cases with headlines and owners; adapt framing from dashboards for public health leaders.
- Short briefs for decisions using the structure in AI‑assisted evidence synthesis for policy briefs.
Equity at the integration layer
Stratify integrated outputs by language, race/ethnicity (when collected), payer, neighborhood, and rurality. Track coverage (who appears in integrated views) and outcomes by subgroup. For outreach lists, reuse fairness checks from AI for population health management and ensure interpreter‑first scripts where needed.
Case vignette: integrating maternal signals
Goal: catch postpartum hypertension risks earlier and target support.
- Sources: EHR vitals and meds; registry outcomes; program rosters for transport vouchers and interpreter services; vital records for births.
- Matching: deterministic on MRN + date of birth; fuzzy rules for cross‑facility matches; monthly match‑rate reporting.
- Outputs: weekly lists and a dashboard with day‑10 BP completion and severe events—owners listed.
Results: day‑10 completion rises to 67%, severe events fall by 24%, with the largest gains among patients with interpreter need. Findings feed program decisions aligned with AI for population health management.
Common pitfalls (and fixes)
- Big‑bang scope → start with two use cases; expand after wins.
- Unclear owners → assign a product owner and a data steward per dataset.
- Metadata sprawl → define an MVM and keep it current.
- Privacy as paperwork → bake in design choices and test them.
Implementation checklist
- Phrase 2–3 use cases and plain outcomes.
- Map sources and matching rules; report match rates.
- Establish MVM and governance; log access and incidents.
- Deliver early dashboards and briefs with owners and next steps.
- Disaggregate outputs and monitor fairness.
Key takeaways
- Purpose‑built integration beats sprawling data lakes.
- Trust comes from tight metadata, routine quality checks, and privacy by design.
- Deliver early wins; then scale to more use cases.
Sources and further reading
- Interoperability standards (HL7/FHIR) and matching toolkits
- Governance templates for data sharing and processing agreements
- Case studies of integrated data improving prevention and policy